First, CCSVI Alliance, the 501(c)(3) non-profit organization that I volunteer for, had some good media coverage. Check out this link. Doesn’t their president, Sharon Richardson, look soooo presidential? Second, my friend Marc Stecker, aka Wheelchair Kamikaze, is featured on the cover story in the Fall 2010 edition of Momentum magazine, seen here. If you’re one… Continue reading Media Coverage
Tag: CCSVI
CCSVI Diagnosis and Treatment Log Entry #9 – 12 Week Update
Everyone wants to know how I’m doing after my CCSVI procedure. The answer is…I feel exactly the same as I did before my visit to Dr. Sclafani. That may sound like bad news, but maybe it is, and maybe it isn’t. Some people are personally invested in my outcome because they know me and care… Continue reading CCSVI Diagnosis and Treatment Log Entry #9 – 12 Week Update
CCSVI- Diagnosis and Treatment Log Entry #8- My Final Thoughts
(Photo credit: Wikipedia) The world is a tragedy to those who feel, but a comedy to those who think. – Horace Walpole My journey through CCSVI self-education, diagnosis, and treatment has been one of the most remarkable experiences of my life, whether or not I ever see any benefit from it. So with all that… Continue reading CCSVI- Diagnosis and Treatment Log Entry #8- My Final Thoughts
CCSVI- Diagnosis and Treatment Log Entry #7
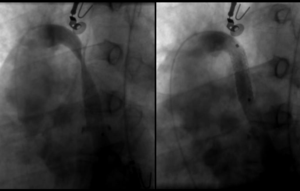
In Log Entry #6 I wrote about what the experience was like for me during the actual CCSVI procedure. Here, in Log Entry #7, I’ll get into the details about the abnormalities that were found, and the actions taken to correct them. To catch up on my complete CCSVI Diagnosis and Treatment log, click here (and… Continue reading CCSVI- Diagnosis and Treatment Log Entry #7
CCSVI- Diagnosis and Treatment Log Entry #6
“Life is either a daring adventure or nothing.” Helen Keller I can’t recall the precise moment when I decided that CCSVI was a legitimate theory about the root cause of MS. Probably it was in October of 2009. I was influenced, like so many of us are, by my friend the Wheelchair Kamikaze. If he… Continue reading CCSVI- Diagnosis and Treatment Log Entry #6
CCSVI- Diagnosis and Treatment Log Entry #5
Just a short note to let everyone know that today’s procedure went well. Dr. Sclafani successfully used angioplasty on both of my jugular veins and my azygos vein. I have a meeting with him tomorrow where I’ll get more details on just how severe the stenosis was. I’m in my hotel room now, and expect… Continue reading CCSVI- Diagnosis and Treatment Log Entry #5
CCSVI- Diagnosis and Treatment Log Entry #4
I have a couple of hours to kill before I leave for the hospital this morning for my CCSVI venogram and possible angioplasty, so I thought I’d blog for a few minutes. I was critical of MRV’s and ultrasounds in my post last night. Let me qualify that a little bit. For someone in my… Continue reading CCSVI- Diagnosis and Treatment Log Entry #4
CCSVI- Diagnosis and Treatment Log Entry #3
The most exciting phrase to hear in science, the one that heralds new discoveries, is not ‘Eureka!’ (I found it!) but ‘That’s funny …’ – Isaac Asimov If yesterday showed King’s County Hospital Center at its worst- slow service, confusion, piles and piles of sometimes redundant paperwork- then today revealed the hospital at its… Continue reading CCSVI- Diagnosis and Treatment Log Entry #3
CCSVI- Diagnosis and Treatment Log Entry #2
Today was a day of hurry up and wait. Nothing accomplished other than paperwork, etc. Tomorrow should be busy with MRV, Ultrasound, and consults. It’s late, and today was uneventful, so this post will be short. Why is it late, you ask? Well, Kim and I went to dinner in Manhattan with a group that… Continue reading CCSVI- Diagnosis and Treatment Log Entry #2
CCSVI- Diagnosis and Treatment Log Entry #1
(Photo credit: Wikipedia) As I indicated in my previous post, this is my CCSVI week- diagnosis and hopefully treatment. I plan to update this blog frequently with details of my adventure. This post is installment #1. My lovely wife and I made the trek from Maine to our hotel room- a 5 hour drive without… Continue reading CCSVI- Diagnosis and Treatment Log Entry #1